How often have you forgotten about a doctor’s appointment until you received a text message reminder?
For people who rely on social services benefits — e.g., the Supplemental Nutrition Assistance Program (SNAP); SNAP for Women, Infants & Children (WIC); Temporary Assistance for Needy Families (TANF); and Medicaid — reminders about appointments and deadlines aren’t just a convenience.
They can mean gaining or maintaining access to critical programs. They also can avoid a phenomenon called “churn,” in which people inadvertently lose, and then quickly regain, benefits because they neglected to renew them or encountered other procedural troubles.
People often learn that they’ve lost benefits when they try to access them and fail — when a health care provider suddenly declines their insurance or their Electronic Benefits Transfer card is unexpectedly empty, for instance. Reapplying for a social services program is more stressful and burdensome than processing a simple renewal.
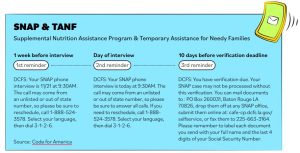
To keep beneficiaries on track, improve customer experience (CX) and bypass largely ineffective hard-copy reminders, some agencies now use one-way text message campaigns to remind people about filing deadlines, submission requirements, appointments, events and other program concerns.
For example, in Louisiana, a pilot project called LA’MESSAGE broadcasts text reminders to people at key stages in a benefit program’s enrollment and renewal process. In developing the project, officials collaborated with low-income Louisianans to learn what information and language they’d value.
Data indicates that LA’MESSAGE has reduced churn, often dramatically. More than 9,900 Medicaid renewal clients increased their annual case approval rate by 67%, and more than 750 WIC clients improved their kept appointment rate by 79%, among other achievements.
This article appears in our guide “How to Change Things up (and Make It Stick).” To read more about ways to innovate successfully, download it here:




Leave a Reply
You must be logged in to post a comment.